Duplex ultrasound investigation of the veins in chronic venous disease Anatomy UIP Part II Anatomy

Duplex ultrasound investigation of the veins in chronic venous disease Anatomy UIP Part II Anatomy
Objectives : Duplex ultrasound investigation has become the reference standard in assessing the morphology and haemodynamics of the lower limb veins. The project described in this paper was an initiative of the Union Internationale de Phlebologie (UIP), The aim was to obtain a consensus of international experts on the methodology to be used for assessment of anatomy of superficial and perforating veins in the lower limb by ultrasound imaging.
Design : Consensus conference leading to a consensus document.
Methods : The authors performed a systematic review of the published literature on duplex anatomy of the superficial and perforating veins of the lower limbs; afterwards they invited a group of experts from a wide range of countries to participate in this project. Electronic submissions from the authors and the experts (text and images) were made available to all participants via the UIP website. The authors prepared a draft document for discussion at the UIP Chapter meeting held in San Diego, USA in August 2003. Following this meeting a revised manuscript was circulated to all participants and further comments were received by the authors and included in subsequent versions of the manuscript. Eventually, all participants agreed the final version of the paper.
Results : The experts have made detailed recommendations concerning the methods to be used for duplex ultrasound examination as well as the interpretation of images and measurements obtained. This document provides a detailed methodology for complete ultrasound assessment of the anatomy of the superficial and perforating veins in the lower limbs.
Conclusions : The authors and a large group of experts have agreed a methodology for the investigation of the lower limbs venous system by duplex ultrasonography, with specific reference to the anatomy of the main superficial veins and perforators of the lower limbs in healthy and varicose subjects.
Introduction
Duplex ultrasound is widely used to investigate chronic venous disease of the lower limbs. In recent years, there has been a much better understanding of the ultrasound images of superficial veins and how these relate to venous disease. A recent publication following a consensus meeting held during the UIP Congress in Rome, September 20011 detailed the nomenclature to be used for superficial and deep veins. The following document results from a further consensus meeting of experts in ultrasound imaging during the UIP Congress in San Diego, August 2003. The aims are to agree about the anatomy of the superficial venous system of the lower limbs in health and disease as shown by ultrasound, and to define the best techniques for imaging.
Methodology
The UIP invited three chairmen (AC, PCS, NL) to prepare a list of international experts in the field of venous duplex ultrasound. They were invited to submit literature references and written contributions that encapsulated important aspects of clinical practice and interpretation of duplex ultrasound images of the venous system of the lower limb. They provided personal opinions that did not necessarily reflect policies of scientific or medical societies to which they may have been affiliated. The literature references provided during this process were not intended to form a systematic review of the literature but were selected to support statements made in the final document where evidence exists. The Consensus Group concentated on publications concerning the interpretation of duplex ultrasound images since there is very little published data comparing anatomical dissections with ultrasound images of the venous system of the lower limb. The authors acknowledge that many of the statements concern subjects which have not been the subject of detailed scientific study and reflect the personal experience of the Consensus Group. The organising committee prepared a draft document that was placed on the UIP website for further discussion, submissions and recommendations. The experts and organising committee met at the Congress in San Diego to discuss the draft document and make further submissions. A further draft was then circulated to all contributors to obtain their comments prior to presenting the final consensus. A more detailed methodology and rationale is included in Part 1 of this consensus document.
Anatomy
Introduction
Venous anatomy is very variable in some parts but more constant in other parts of the lower limbs. Common variations in lower limb venous anatomy are described in this section, for it is necessary to understand them correctly to identify veins and diagnose disease using ultrasound imaging.
In the past, a wide range of terms including eponymous names was used to describe lower limb veins. A recent publication by Caggiati et al.1 unified terminology and definitions for the venous system with particular reference to the lower limb, and the present consensus is based on that presentation. It uses English terms to describe veins rather than less generally used Latin terms or eponymous nomenclature.
The following section defines the main ultrasound markers of anatomy of the veins of the lower limbs, according to the published literature, and the anatomy of each vein considered to be relevant for clinical practice and for research in venous disease is presented. Later, the document discusses in detail anatomical variations that have been reported in thepublished literature.
Haut de page Ultrasound markers of venous anatomy
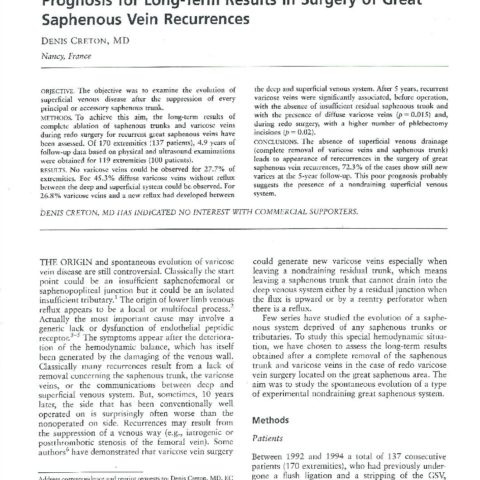
The saphenous eye
Ultrasound appearances identify the main saphenous trunks within their fascial compartments. Bailly2 was the first to describe the ‘eye sign’ to identify the GSV in the thigh by ultrasound. A more detailed description of the saphenous compartment has been published more recently.3,4 The sign is due to the fact that superficial fascia is echogenic and easily observed on ultrasound (Fig. 1). The compartment in which the saphenous trunks run resembles an ‘Egyptian eye’ in a transverse scan where the saphenous lumen is the iris, the superficial fascia the upper eyelid, and the aponeurotic deep fascia the lower eyelid. The deep layer arises from the muscle fascia and is usually better defined than the superficial or saphenous fascia. The ‘eye’ sign is always present and allows the saphenous vein to be clearly identified and distinguished from parallel subcutaneous tributaries.
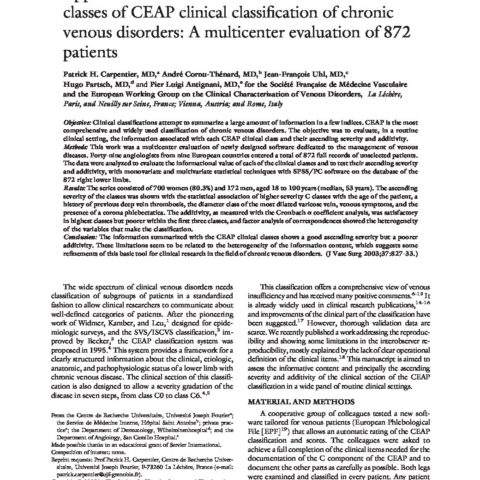
Alignment sign
The great saphenous vein (GSV) and the anterior accessory saphenous vein (AASV) frequently form two ‘saphenous eyes’ in the upper third of thigh on a transverse ultrasound scan. The image clearly distinguishes the GSV from the AASV since the AASV lies anterior and lateral to the GSV over (aligned with) the femoral artery and vein2 (Fig. 2). In some limbs, the alignment sign shows that the only vein visible as an ‘eye’ is the AASV since the GSV is not visible (absent or hypoplastic).5
Tibio–gastrocnemius angle sign
The location of the GSV relative to the tibia and medial gastrocnemius muscle below the knee on ultrasound allows it to be distinguished from a tributary of the GSV.6 The GSV in the knee area is distinguished from nearby veins by its position on a transverse scan in the triangle formed by the tibia, medial gastrocnemius muscle and fascial sheet (Fig. 3). This sign identifies the GSV below knee where fascial sheets are often so close to each other that the compartment in which the GSV runs may be difficult to recognise. If the saphenous space is empty, this indicates that the GSV is absent or hypoplastic.
Tributaries
Tributaries run parallel or beside the track of the associated saphenous vein but are not situated within a saphenous eye on ultrasound imaging. A tributary may be the main axial superficial vein but is not regarded as a saphenous trunk since it lies outside the saphenous compartment3,5,7 (Fig. 4).
Anatomy of the superficial venous system
Saphenous veins and junctions
GSV-great saphenous vein : The term great saphenous vein (vena saphena magna) abbreviated as GSV should be used instead of terms such as long, greater or internal saphenous vein. It is recommended to avoid the term ‘long saphenous vein’ to prevent confusion caused by the abbreviation LSV which could refer to either the long saphenous or lesser saphenous vein.
SFJ-saphenofemoral junction : The saphenous vein terminates at the SFJ. The SFJ is at the level of the groin skin crease and is covered by superficial fascia that ends proximally at the inguinal ligament. The terms ‘confluence of superficial inguinal veins’ (confluens venosus subinguinalis), also known as the ‘crosse’ by many clinicians, or the Venenstern unter dem Leistenband of German anatomists, correspond to the veins of the SFJ.
AASV-anterior accessory saphenous vein : The anterior accessory saphenous vein (vena saphena magna accessoria anterior) refers to a venous segment ascending parallel to the GSV in the thigh and located anteriorly within a fascial compartment in the thigh shown by ultrasound to have its own saphenous compartment.
PASV-posterior accessory saphenous vein : The posterior accessory saphenous vein (vena saphena magna accessoria posterior) refers to a venous segment ascending parallel to the GSV and located posteriorly, shown by ultrasound to be contained within a fascial compartment in the thigh. This vein is not found as often as the AASV and its connection with GSV is not constant.
SSV-small saphenous vein : The term small saphenous vein (vena saphena parva) abbreviated as SSV should be used instead of short, external, or lesser saphenous vein. The small saphenous vein passes between the heads of gastrocnemius and frequently terminates by joining the popliteal vein in the popliteal fossa.
SPJ-saphenopopliteal junction : The SPJ is the termination of the SSV with the popliteal vein. This most often lies 2–4 cm above the popliteal skin crease8 but its exact location is variable.
TE-the thigh extension of the small saphenous vein : This vein (extensio cranialis venae saphenae parvae) courses in the groove between the biceps femoris and semimembranosus muscles. It has been called the ‘femoropopliteal vein’ or cranial extension of the SSV and it terminates in one or more superficial or perforating veins of the thigh or gluteal region but not in the GSV. A cranial extension of the SSV or TE of SSV that communicates with the GSV via the posterior thigh circumflex vein is termed the vein of Giacomini (GV).
Venous tributaries
Lateral venous system : The lateral venous system (sistema venosa lateralis membri inferioris or Albanese system) is on the lateral thigh and leg and may represent the remnant of the embryonic lateral marginal vein (vena marginalis lateralis).
The anterior thigh circumflex vein : The anterior thigh circumflex vein (vena circumflexa femoris anterior) is a tributary of the GSV or AASV that ascends obliquely in the anterior thigh. It may originate from the lateral venous system.
The posterior thigh circumflex vein : The posterior thigh circumflex vein (vena circumflexa femoris posterior) is a tributary of the GSV or PASV which ascends obliquely in the posterior thigh. It may originate in the SSV, its thigh extension, or the lateral venous system.
Intersaphenous veins : One or more intersaphenous vein(s) [vena(e) intersaphena(e)] course obliquely in the leg to connect the SSV and GSV.
Anatomy in the great saphenous venous territory
The GSV commences its course anterior to the medial malleolus and passes upwards along the tibial edge of the medial calf to cross the knee and then along the medial thigh to the SFJ. The GSV has a constant terminal valve 1–2 mm distal to the SFJ, which is usually easily identified on duplex ultrasound.9 There is often another pre-terminal valve a further 2 cm distal, which marks the distal limit of the SFJ area9 (Fig. 5). The most important tributaries join the GSV between the two valves, and these veins are fairly constant and readily identified by ultrasound. These tributaries are proximal or distal.
Proximal veins drain venous blood from the abdominal wall and pudendal areas, and from lateral to medial. These are the superficial circumflex iliac, superficial epigastric and superficial external pudendal veins. Proximal veins may be single or multiple and are of clinical importance because they may transmit retrograde flow into the GSV even with a competent terminal valve, reported in 28–59% of cases.9–11
Distal merging veins at the SFJ are often relatively large and are typically the lateral AASV which is present in 41% of subjects12 joining the GSV within 1 cm of the SFJ, and the medial PASV which may represent the proximal end of the Giacomini vein at a variable distance from the SFJ, often distal to the preterminal valve. In most cases, there is a quite constant lymph node in the angle between the GSV and AASV before they merge and the vein net of lymphaticnode(s) that surrounds the AASV may be sometimes large and incompetent, forming a source for reflux into thigh and leg varicose veins.13
The anterior accessory saphenous vein
Close to the SFJ, the GSV medially and the AASV laterally often lie within the same saphenous compartment. More distally, the AASV has its own ‘eye’ and is distinguished from the GSV by the ‘alignment’ sign, and with an anterolateral course in the thigh.
Some authors have reported different frequencies for the AASV associated with the GSV14–16 as well as anatomical variations in the diameter, length and course of the AASV, and relevant tributaries outside the compartment, described by duplex scanning.12 The AASV is involved in about 14% of patients with varicose veins,12 and if so then the AASV may be the only proximal source for reflux while the GSV is competent, or alternatively there may be reflux in both the GSV and AASV.
Relation of fascial compartments to the GSV and anatomical variations in the thigh
In the thigh, the GSV is contained in its ‘saphenous eye’.4 The fascial compartment is larger and better defined in the thigh than in the leg. Tributaries pierce the superficial layer of fascia to reach the GSV. Transverse ultrasound imaging of the GSV territory in the thigh based on the ‘eye’ sign has revealed the following anatomical patterns.7
- (A) A single GSV lying within the saphenous compartment with no large parallel tributary.
- (B) The GSV in the thigh comprising two parallel veins, both lying within the saphenous compartment for a distance of 3–25 cm. (true GSV duplication), which is present in less than 1%.17
- (C) A single GSV lying within the saphenous compartment as well as a large subcutaneous tributary that pierces the superficial fascia to join the GSV at a variable level in the thigh.
- (D) Two veins, the GSV and AASV, both present in the thigh, located distally in two separate ‘saphenous eyes’ coming together in a single compartment just before entering the SFJ area In many cases, the AASV is incompetent filling varicosities over the anterior and lateral aspects of the thigh.
- (E) A single GSV lying within the proximal saphe nous compartment as well as a large subcu taneous tributary more distally with no substantial vein visible in the saphenous compartment. The distal subcutaneous vein pierces the saphenous fascia at a variable level in the thigh to become the GSV within the fascial compartment.
Relation of fascial compartments to the GSV and anatomical variations at the knee
It may be difficult to recognise the GSV and its fascia forming the ‘saphenous eye’ near the knee using ultrasound, and the GSV can be confused with a number of subcutaneous tributaries and perforating veins confined within a small space in the region. The GSV can be identified from transverse ultrasound images by the tibio–gastrocnemius angle sign between the distal third of thigh and proximal third of calf.
This ultrasound sign has been described in subjects with and without varicose veins. Five patterns (A–E) have been reported6 (Fig. 6)
- (A) The GSV is visible and no large tributary is seen.
- (B) The GSV is visible but there are one or more tributaries below the knee the most typical being the posterior arch or ‘Leonardo’ vein.
- (C) The GSV is visible, but there is also a large tributary that begins above the knee, which whether normal or varicose, is sometimes so large that it may be erroneously assumed to be the GSV itself. The GSV is always present in the knee area in all of the three patterns described above (A–C) though sometimes smaller than its normal or varicose tributaries. In contrast the middle portion of the GSV is barely visible or not visible at all (hypoplastic or absent) for a variable length in about 30% of cases with the ‘missing’ portion bypassed by a subcutaneous tributary.
Two patterns are observed: - (D) The GSV cannot be demonstrated for some distance above and below knee. The GSV pierces the saphenous fascia at about the mid-calf to become a subcutaneous tributary, which crosses the knee and again pierces the saphenous fascia in the distal thigh to become the GSV in its saphenous compartment.
- (E) This is similar to ‘D’ but the absent portion of the GSV is very short and just below rather than across the knee.
This classification of GSV patterns at the knee cannot be applied in 3% of cases.
The study reported above6 showed that varicose veins were present in 34% of limbs where the GSV was present throughout the thigh and calf (types A–C) and in 56% of limbs with the patterns where a segment of GSV was missing at the knee (types D and E).
Relation of fascial compartments to the GSV and anatomical variations in the leg
The GSV is nearly always present from the medial malleolus to the level of the mid-calf paratibial perforator. The saphenous fascia is very strong in the leg and the saphenous compartment compressed between tibia and muscles is very narrow. These factors together with the substantial thickness of the saphenous wall mean that the distal GSV is rarely dilated or incompetent.6,18 There are usually one or more subcutaneous tributaries lying parallel to the GSV in the distal calf.
Relations between the GSV and tributaries
The GSV both in the leg and in the thigh is often accompanied by parallel veins of different length that are so large that they may be confused with the GSV itself or considered to be ‘double’ saphenous veins. Ultrasound imaging shows that these veins are not a duplication of the GSV but are tributaries lying subcutaneously that may then pierce the superficial fascia to enter the saphenous compartment. The relationship between the GSV and these subcutaneous tributaries may be classified as three anatomical patterns, each with a specific ultrasound appearance7 (Fig. 7):
- Type ‘I’: the saphenous trunk is present with a normal diameter throughout the length of the saphenous compartment and there are no large parallel tributaries.
- Type ‘h’: the saphenous trunk is present throughout the saphenous compartment, and there is also a tributary vein that may be even larger than the GSV.
- Type ‘S’: a superficial tributary ascends and pierces the superficial fascia continuing as the GSV within its compartment, while distal to this point the GSV is absent or only barely visible on ultrasound imaging (absent or hypoplastic).
Anatomy in the small saphenous venous territory
The small saphenous vein (SSV) begins behind the lateral malleolus as a continuation of the lateral marginal foot vein. It ascends the posterior aspect of calf and frequently terminates at the popliteal vein. The SSV lies for its entire length in an interfascial compartment defined by the deep muscular fascia and superficial fascia. The distal compartment appears on a transverse ultrasound scan as an ‘eye’ similar to that for the GSV in the thigh. The proximal compartment is typically triangular and defined by the medial and lateral heads of the gastrocnemius muscle and the superficial fascia that stretches over the intermuscular groove. The SSV is occasionally duplicated with two or even three veins of various lengths running in its compartment.
The saphenopopliteal junction—anatomical variations
There are three patterns at the SSV termination (Fig. 8):
- (A) The SSV joins the popliteal vein at the saphenopopliteal junction (SPJ) and joins deep veins at a higher level through its TE or joins GSV via Giacomini vein (Fig. 8(A1) and (A2)).
- (B) The SSV continues upwards as TE or GV, but it also connects with popliteal vein through an ‘anastomotic’ tiny vein.
- (C) There may be no connection to deep veins so that the SSV continues proximally as the TE or vein of Giacomini.
The saphenopopliteal junction (SPJ) is most often situated within 5 cm of the popliteal skin crease. However, its level is variable, most often at 2–4 cm above the knee crease, higher than this level in 25%, and rarely below the knee crease.8 A recent metanalysis19 showed that a higher location of SPJ (i.e. more than 7 cm above the popliteal line) is common (up to 46.6%) in healthy subjects, whereas in case of incompetence of the SPJ this is located in the vast majority of the cases (57–93.7%) within the popliteal fossa (0–7 cm above the popliteal line).
One study showed that the SSV joined the popliteal vein on the posterior aspect in 15%, posteromedial in 30%, posterolateral in 12% lateral in 42%, or even anterolateral in 1% of limbs.20 The terminal part of the SSV includes two valves : the terminal one, which is in close proximity with the popliteal vein (Fig. 5), and the pre-terminal one, which is usually located below the depart of Giacomini vein or of the TE of SSV.
Gastrocnemius veins may join the popliteal vein, upper SSV, or their confluence at the SPJ. The SSV may merge with the gastrocnemius veins before joining the popliteal vein, in 10–30% of limbs.20–23
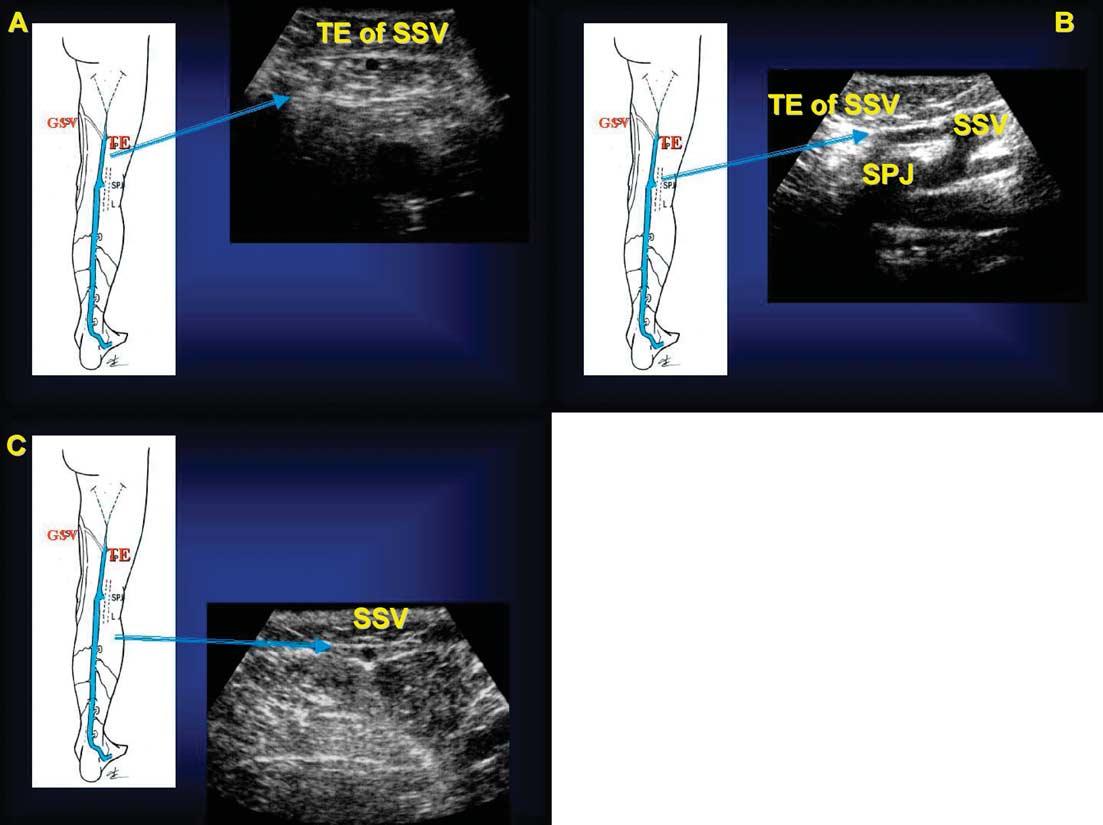
Thigh extension (TE) of the SSV
In 1873, Giacomini described the TE and its frequent connection to the GSV. Further anatomical dissections24,25 confirmed that the SSV usually extends into the thigh. The anatomy of the TE has been confirmed by ultrasound imaging.26–28 The TE of the SSV is present in 95% of limbs27 and lies deep to the fascia on the back of the thigh. The distal TE is recognised on ultrasound by its intrafascial position into a triangleshaped compartment that resembles the saphenous compartment for the SSV, and is defined by the semitendinosus muscle medially, the long head of the biceps muscle laterally and the superficial fascia that stretches over the intermuscular groove (Fig. 9).
Various terminations have been described.29 The proximal TE may :
- (A) continue straight up into the gluteal area as a single vein or divided in many deep and superficial branches
- (B) join the deep femoral veins as a posterior or posterolateral thigh perforator
- (C) divide into many muscular or subcutaneous branches of the posterior thigh
- (D) connect to the posterior thigh circumflex vein which then passes to the GSV in the medial thigh, this complex of veins (TE of SSVCposterior thigh circumflex vein) being termed the vein of Giacomini.
In many cases, the proximal limit of the TE is a combination of the above terminations.
The TE and Giacomini vein may transmit reflux from proximal incompetent veins (e.g. GSV, perineal veins, thigh perforators) to the SSV, or, vice versa, may transmit an ‘ascending reflux’ from SPJ upwards to GSV and/or varicose veins of the posterior aspect of the thigh.30
Arrangement of the SSV and its tributaries
Subcutaneous tributaries of the SSV and TE are recognised because they pierce the superficial fascia to enter the saphenous compartment and join the SSV or TE trunk.
One particular tributary that deserves separate description is the so-called ‘popliteal fossa perforating vein’ and was described first by Dodd.31,32 This vein runs subcutaneously along the posterior aspect of the calf and popliteal area; sometimes parallel to the SSV and typically forms a separate junction with the popliteal vein usually lateral to the SPJ.
Anatomy of perforating veins
Perforating veins connect deep veins with superficial veins and may be single- or multiple-branched; duplex anatomy is characterized by their penetration through the muscular fascia. Perforating veins are numerous and very variable in arrangement, connections, size, and distribution. More than 40 constantly present perforating veins have been described.33 In clinical practice, perforators have been frequently associated with names of authors, often incorrectly from a historical point of view, which is sometimes mislead- ing. Instead, descriptive terms designating location are preferred. Perforators are grouped on the basis of their topography.1,33
Perforators of the foot (venae perforantes pedis) are divided into dorsal, medial, lateral and plantar foot perforators.
Ankle perforators (venae perforantes malleolaris) are designated as medial, anterior and lateral ankle perforators.
Perforators of the leg (venae perforantes cruris) are divided into four main groups
- (a) Medial leg perforators are designated as paratibial or posterior tibial. Paratibial perforators (formerly Sherman perforators in the lower and mid leg and Boyd perforators in the upper leg) connect the main GSV trunk or its tributaries with the posterior tibial veins or calf muscle plexus and lie close to the medial surface of the tibia. Posterior tibial perforators (formerly Cockett perforators) connect the posterior arch vein with the posterior tibial veins. They should not be named first, second, and third but are better indicated topographically as upper, middle, and lower.
- (b) Anterior leg perforators pierce the anterior tibial compartment fascia to connect anterior GSV tributaries to the anterior tibial veins.
- (c) Lateral leg perforators connect veins of the lateral venous plexus with the peroneal veins.
- (d) Posterior leg perforators are divided into medial gastrocnemius perforators in the medial calf, lateral gastrocnemius perforators in the lateral calf, intergemellar (soleal) perforators connecting the SSV with soleal veins (formerly the mid-calf perforator of May), and para-Achillean perforators connecting the SSV with the peroneal veins (formerly perforator of Bassi).
Perforators of the knee (venae perforantes genus) are designated as medial or lateral knee perforators, suprapatellar or infrapatellar perforators, and popliteal fossa perforators.
Perforators of the thigh (venae perforantes femoris) are grouped according to their position. On the medial thigh are perforators of the femoral canal (formerly named Dodd perforators) and inguinal perforators, which connect the GSV or its tributaries with the femoral vein. Anterior thigh perforators pierce the quadriceps femoris. Lateral thigh perforators pierce the lateral muscles of the thigh. Posterior thigh perforators are designated as posteromedial thigh perforators piercing the adductor muscles, sciatic perforators lying along the midline of the posterior thigh, posterolateral thigh perforators piercing the biceps femoris and semitendinosus muscles (formerly Hach perforators), and pudendal perforators. Perforators of the gluteal muscles (venae perforantes glutealis) are divided in superior, mid, and lower perforators.
Anatomy of foot veins
The arrangement of superficial foot veins is in two layers separated by the superficial fascia as in the rest of the limb and this can be demonstrated by ultrasound.34 The dorsal venous arch and the medial and lateral marginal veins are the anatomic origins of the GSV and SSV and are placed under the superficial fascia; tributaries on the dorsum of the foot pass upwards to become subcutaneous tributaries of the leg above the superficial fascia. Varicose veins in the medial and lateral retromalleolar space are also subcutaneous tributaries of the GSV and SSV, respectively.
Conclusions
This description of lower limb venous anatomy demonstrated by ultrasound imaging is intended to be the basis for future research regarding the morphology of healthy and diseased superficial and perforating veins. We believe that publishing this description will help us to reach agreement on how veins of the lower limbs change in various disease states. A clear understanding of anatomy helps to select and perform the best treatment for the patient.
Acknowledgements
List of the experts who were invited to review this document in S. Diego during the Consensus Meeting, or via internet : Allegra Claudio (ITA), Antignani P. Luigi (ITA), Bergan John (USA), Bradbury Andrew (GBR), Caggiati Alberto (ITA), Cappelli Massimo (ITA), Cavezzi Attilio (ITA), Chunga Chunga Juan (PER), Coleridge-Smith Philip (GBR), Creton Denis (FRA), De Simone Juan (ARG), Franceschi Claude (FRA), Gallenkemper Georg (GER), Georgiev Mihael (ITA), Grondin Louis (CAN), Guex J. Jerome (FRA), Jaeger Kurt (SWI), Jeanneret Christina (SWI), Kabnick Lowell (USA), Labropoulos Nicos (USA), Lindhagen Anders (SWE), Marshall Markward (GER), Morrison Nick (USA), Myers Ken (AUS), Nelzen Olle (SWE), Nicolaides Andrew (CYP), Partsch Hugo (AUT), Pereira Alves Carlos (POR), Pichot Olivier (FRA), Pieri Alessandro (ITA), Rabe Eberhard (GER), Raymond-Martimbeau Pauline (CAN), Ricci Stefano (ITA), Rilantono Lily I (Indonesia), Schadeck Michel (FRA), Scuderi Angelo (BRA), Somjen George M (AUS), Staelens Ivan (BEL), Strejcek Jaroslav (CZR), Tessari Lorenzo (ITA), Thibault Paul (AUS), Uhl J. Francois (FRA), Van Rij Andre (NZL), Von Planta Irene (SWI), Weiss Robert (USA), Zamboni Paolo (ITA).
The authors express their gratitude to Pierluigi Antignani (webmaster of the UIP website) and to Bernhard Partsch (secretary of the working group) for their collaboration.
References
- Caggiati A, Bergan JJ, Gloviczki P, Jantet G, Wendell-Smith CP, Partsch H. Nomenclature of the veins of the lower limbs : an international interdisciplinary consensus statement. J Vasc Surg 2002;36:416–422.
- BAILLY M, Cartographie CHIVA. Encyclopedie Medico-Chirurgicale. Paris;1993:43–161-B: 1–4.
- Lemasle PH, Uhl JH, Lefebvre-Vilardebo M, Baud JM. Proposition d’une definition echographique de la grande saphene et des saphenes accessoires a l’etage crural. Phlebologie 1996;49:279–286.
- Caggiati A, Ricci S. The long saphenous vein compartment. Phlebology 1997;12:107–111.
- Ricci S, Caggiati A. Does a double saphenous vein exist? Phlebology 1999;14:59–64.
- Ricci S, Cavezzi A. Echo-anatomy of long saphenous vein in the knee region: proposal for a classification in five anatomical patterns. Phlebology 2002;16:111–116.
- Ricci S, Caggiati A. Echoanatomical patterns of the long saphenous vein in patients with primary varices and in healthy subjects. Phlebology 1999;14:54–58.
- Myers KA, Wood SR, Lee V, Koh P. Variations of connections to the saphenous system in limbs with primary varicose veins: a study in 1481 limbs by duplex ultrasound scanning. J Phlebol 2002;2:11–17.
- Pieri A, Vannuzzi A, Duranti A, Vin F, Benalli L, Michelagnoli S et al. Role central de la valvule pre-ostiale de la veine saphene interne dans las genese des varices tronculaires des membres inferieures. Phlebologie 1995;48:227–239.
- Somjen GM, Donlan J, Hurse J, Bartholomew J, Johnston AH, Royle P. Venous reflux at the sapheno–femoral junction. Phlebology 1995;10:132–135.
- Cavezzi A, Carigi V, Collura M. Colour flow Duplex scanning as a preoperative guide for mapping and for local anaesthesia in varicose vein surgery. Phlebology 2000;15:24–29.
- Ricci S, Georgiev M. Ultrasound anatomy of the superficial veins of the lower limb. J Vasc Technol 2002;26:183–199.
- Lemasle P, Uhl JF, Lefebvre-Vilardebo M, Baud JM, Gillot C. Veines lympho-ganglionnaires inguinales. Aspects anatomiques et echographiques. Consequences sur la definition de la neogenese. Consequences therapeutiques. Phlebologie 1999;52(3):263–269.
- Bassi G. Le varici degli arti inferiori: Cap I, pag 19. Edizioni Minerva Medica-Torino; 1962.
- Muller R, Joubert B. La Phlebectomie Ambulatoire: De l’anatomie au geste. Pag 39 Les Editions Medicales Innothera; 1994.
- Davy A, Ouvry P, Guenneguez H. A propos des saphenes anterieures de cuisse. Phlebologie 1985;38:279–291.
- Zamboni P, Cappelli M, Marcellino MG, Murgia AP, Pisano L, Fabi P. Does a varicose saphenous vein exist ? Phlebology 1997;12:74–77.
- Cavezzi A. Diagnostic de l‘insuffisance veineuse superficielle des membres inferieurs par echo-doppler-couleur. Phlebologie 2000;1:15–22.
- Creton D. Saphenopopliteal junctions are significantly lower when incompetent. Embryological hypothesis and surgical implications. Phlebolymphology 2005;48:347–354.
- Lemasle P, Lefebvre-Vilardebo M, Tamisier D, Baud JM. CORNU-THENARD A. Confrontation echo-chirurgicale de la terminaison de la saphene externe dans le cadre de la chirurgie d’exerese. Resultats preliminaires Phlebologie 1995;3:321–327.
- Cavezzi A, Tarabini C, Collura M, Sigismondi G, Barboni MG, Carigi V. Hemodynamique de la jonction sapheno-poplitee: evaluation par echo-doppler couleur. Phlebologie 2002;55(4):309–316.
- De Simone J. Echo-doppler couleur de la crosse commune petite saphene – veines jumelles. Aspects anatomiques et hemodynamiques. Phlebologie 1998;2:169–177.
- Van der Stricht J, Staelens I. Veines musculaires du mollet. Phlebologie 1994;47:135–143.
- Hoffman HM, Staubesand J. Die venosen Abflussverhaeltnisse der Musculus Triceps surae. Phlebologie 1991;20:164–168.
- Caggiati A. Fascial relationships of the short saphenous vein. J Vasc Surg 2001;34:241–246.
- Georgiev M. The femoropopliteal vein. Ultrasound anatomy, diagnosis, and office surgery. Dermatol Surg 1996;22:57–62.
- Georgiev M, Myers KA, Belcaro G. The thigh extension of the lesser saphenous vein: from Giacomini’s observations to ultrasound scan imaging. J Vasc Surg 2003;37:558–563.
- Labropoulos N, Giannoukas AD, Delis K, Kang SS, Mansour MA, Buckman J et al. The impact of isolated lesser saphenous vein system incompetence on clinical signs and symptoms of chronic venous disease. J Vasc Surg 2000;32:954–960.
- Gillot C. Le Prolongement post axial de la petite veine saphene. Etude anatomique. Considerations fonctionnelles. Interet pathologique. Phlebologie 2000;53:295–325.
- Pieri A, Vannuzzi A, Duranti A, Michelagnoli S, Marcelli F, Santini M et al. La valvule pre-ostiale de la veine saphene externe. Phlebologie 1997;50(3):343–350.
- Dodd H. Persistent varicose veins with special reference to the varicose tributaries of the superficial femoral and popliteal veins. Proc R Soc Med 1958;51:817–820.
- Dodd H. The varicose tributaries of the popliteal vein. Proc R Soc Med 1964;57:394–396.
- Van Limborgh J, Hage EW. Anatomical features of those perforating veins of the leg which frequently or infrequently become incompetent. In: May R, Partsch H, Staubesand J, eds. Perforating veins. Munchen: Urban & Schwarzenberg, 1981:49–59.
- Ricci S. Phlebectomie des varices du pied. Phlebologie 2000;53:223–228.
Fig. 1
(A) Transverse B mode ultrasound image of the great saphenous vein (GSV) in the saphenous compartment of the thigh. (B) Position of the ultrasound probe in the thigh.
Fig.2
Anterior accessory saphenous vein (AASV) and the alignment sign. (A) The AASV lies laterally to the GSV and these two veins terminate in a common trunk (SFJ). (B) B-mode ultrasound image of the SFJ. The left image shows the common trunk (SFJ). On the right, 2 cm more distally, the AASV lies laterally to the GSV. Note: the AASV overlies and alligns with the femoral vessels (femoral vein, superficial femoral artery and deep femoral artery) whilst the GSV passes more medially.
Fig. 3
B-mode ultrasound image just below the knee in two different limbs. Tibia (T)–gastrocnemius (G) angle with great saphenous vein inside (A) and without GSV (B) (due to congenital absence or hypoplasia of GSV); a large saphenous tributary is present in image B (circled).
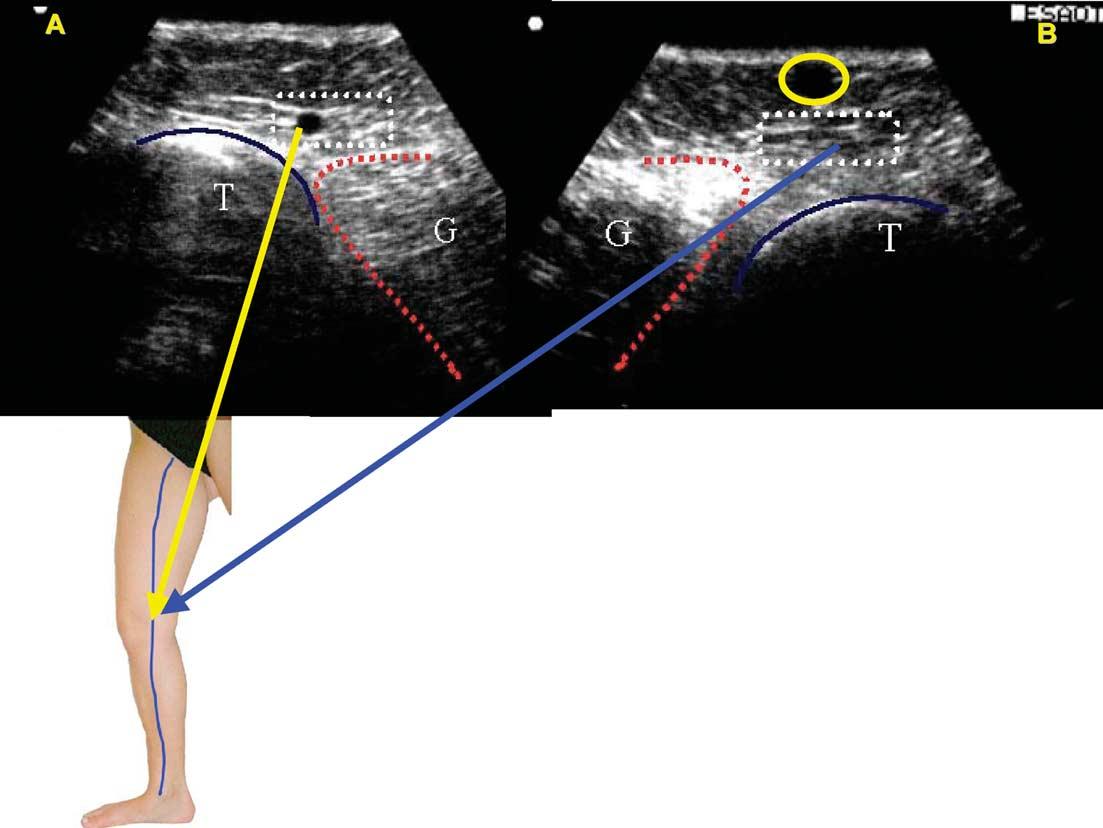
Fig. 4
Relationship between the great saphenous vein and a tributary in the mid thigh area (A) diagram showing the position of the GSV and of its (incompetent) tributary (B) transverse colour-duplex image: left: GSV within the saphenous eye right : (incompetent) tributary above the saphenous fascia and (small, competent) GSV within the saphenous eye (right)
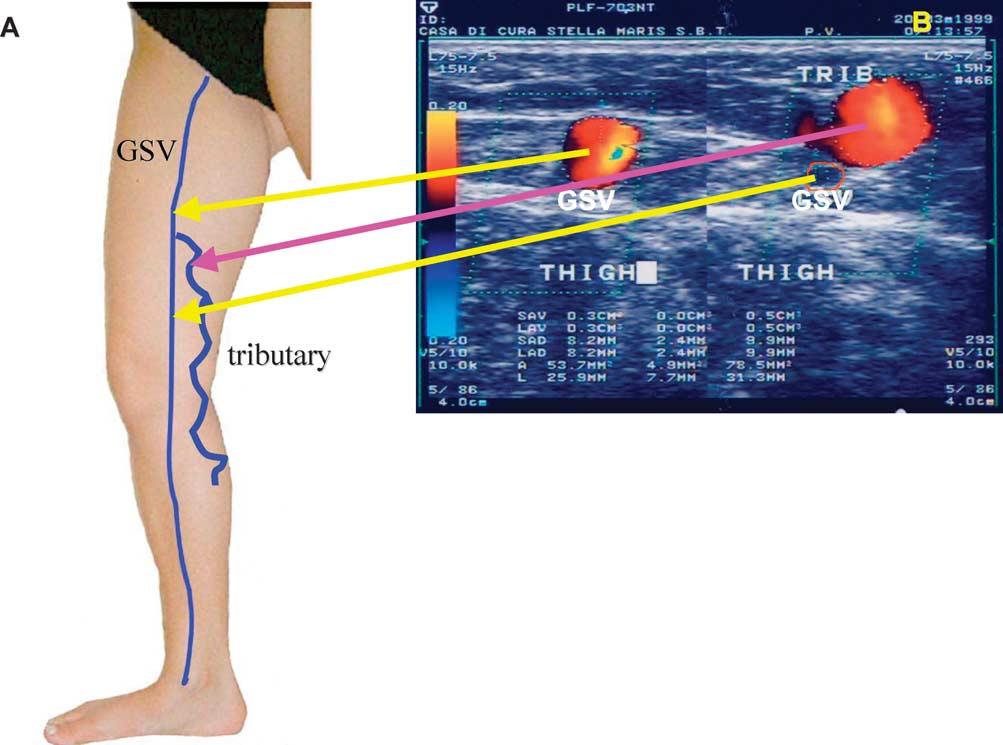
Fig. 5
Great saphenous vein (GSV) and small saphenous vein (SSV) terminal valve (TV) and pre-terminal valve (PTV) (A) saphenofemoral junction and GSV; the arrow on the left indicates TV and the arrow on the right indicates PTV (B) on the left TV during antegrade flow, on the right TV during valsalva manoeuvre (the arrows indicate TV leaflets) (C) saphenopopliteal junction and TV (TERVAL) of SSV close to the popliteal vein (POPV).
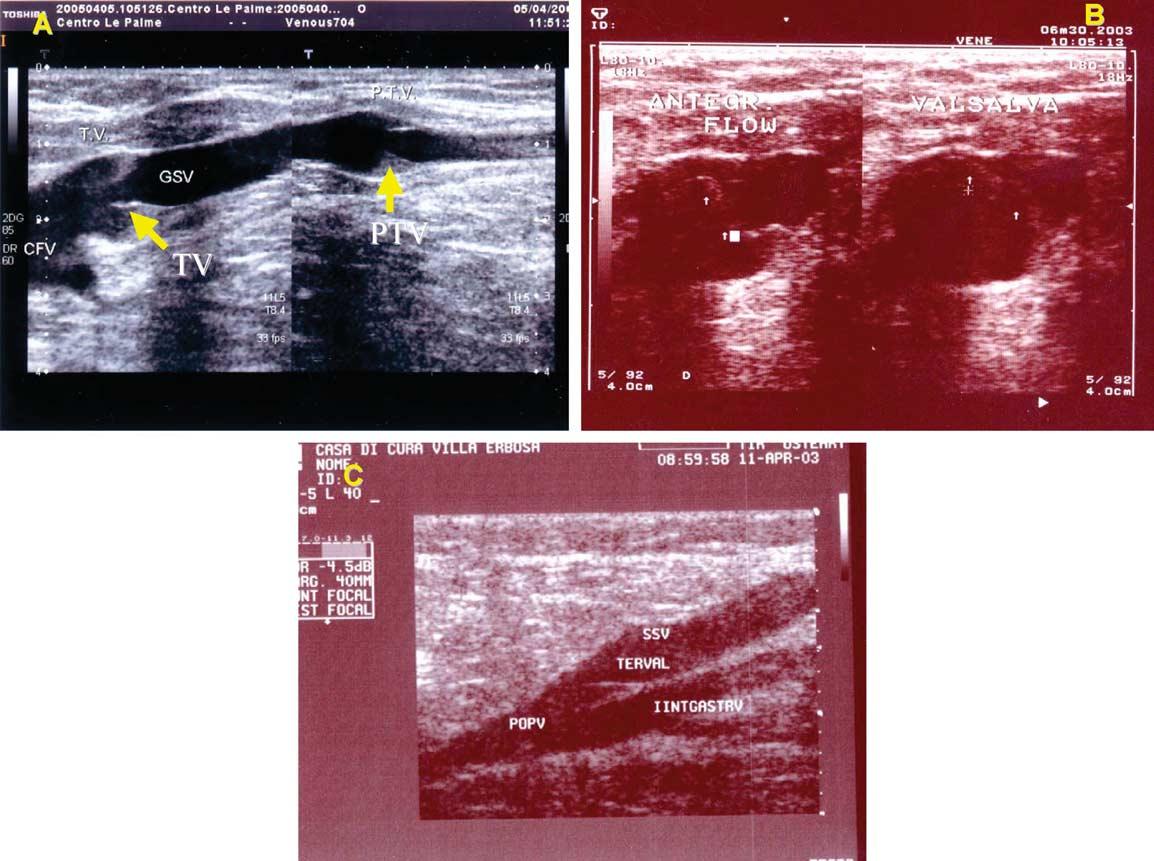
Fig. 6
Relation of fascial compartments to the GSV and anatomical variations at the knee.6
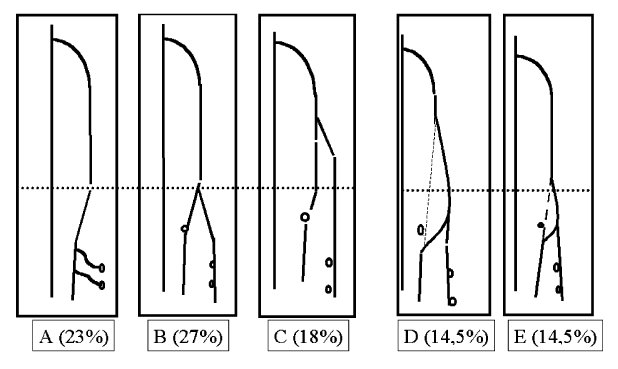
Fig. 7
Relationship between the GSV and tributaries: I, h and S type configurations.
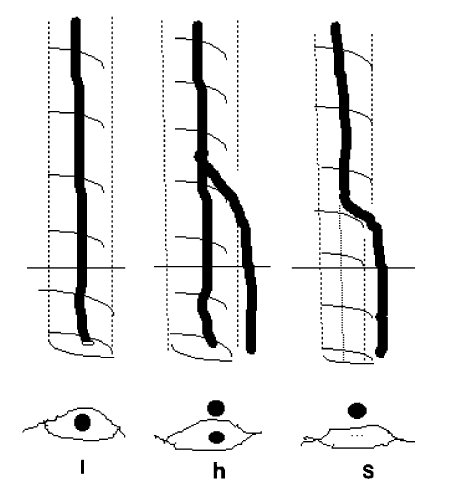
Fig. 8
The saphenopopliteal junction-anatomical variations.
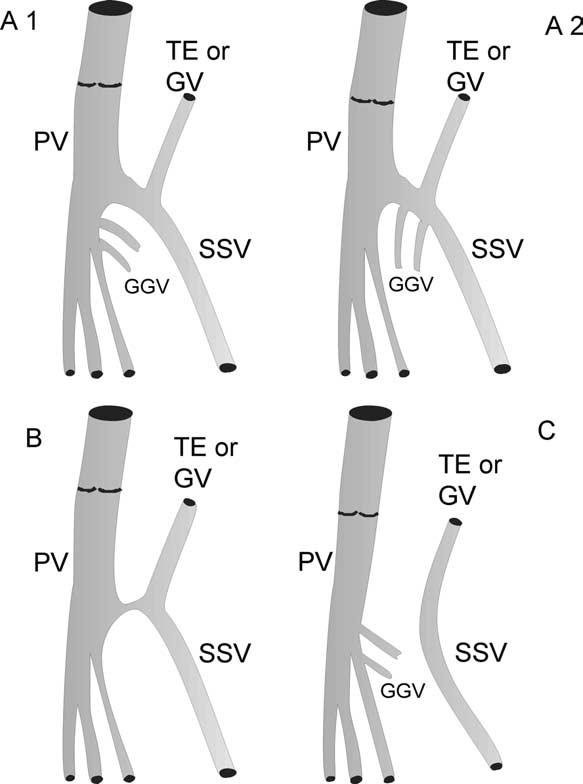
Fig. 9
Transverse scan of the posterior thigh and leg region. Small saphenous vein (SSV) and its thigh extension (TE), both within the saphenous compartment (a) lower third of the thigh (b) saphenopopliteal junction (SPJ) (c) upper third of the leg.
| Date | 2006 |
| Auteurs | Eur J Vasc Endovasc Surg 2006;31:288-99 A. Cavezzi, S. Benedetto del Tronto, Italy; N. Labropoulos, Chicago, IL, USA; H. Partsch, Vienna , Austria; S. Ricci, Rome, Italy; A. Caggiati, Rome, Italy; K. Myers, Melbourne, Australia; A. NicolaidesNicosia, Cyprus; and P.C. Smith Coleridge London, UK; (CRETON D., Nancy, FR; as expert to review) |