Regarding « Ultrasound finding after radiofrequency ablation of the great saphenous vein/ descriptive analysis »
Regarding « Ultrasound finding after radiofrequency ablation of the great saphenous vein/ descriptive analysis »
In the recent article by Sergio Salles-Cunha et al,1 the authors suggest a very high neovascularization rate after radiofrequency ablation (RF) of the great saphenous vein (GSV), which does not correspond to our own experience. The authors describe small vessel networks (SVN), which covers without discrimination all vessels smaller than 2 mm in the surrounding tissue of the treated GSV, including muscular, collateral, and tributary veins and their satellite arteries. The high prevalence of these SVN elements in the groin area and at the thigh level is interpreted as the result of a process similar to the neovascularization described after GSV ligation and stripping. However, without a controlled assessment of the preoperative extent of the SVN, the possibility of pre-existing SVN cannot be excluded, especially when the duplex ultrasound method was not identical before and after surgery, with postoperative setting optimization meant to maximize sensitivity.
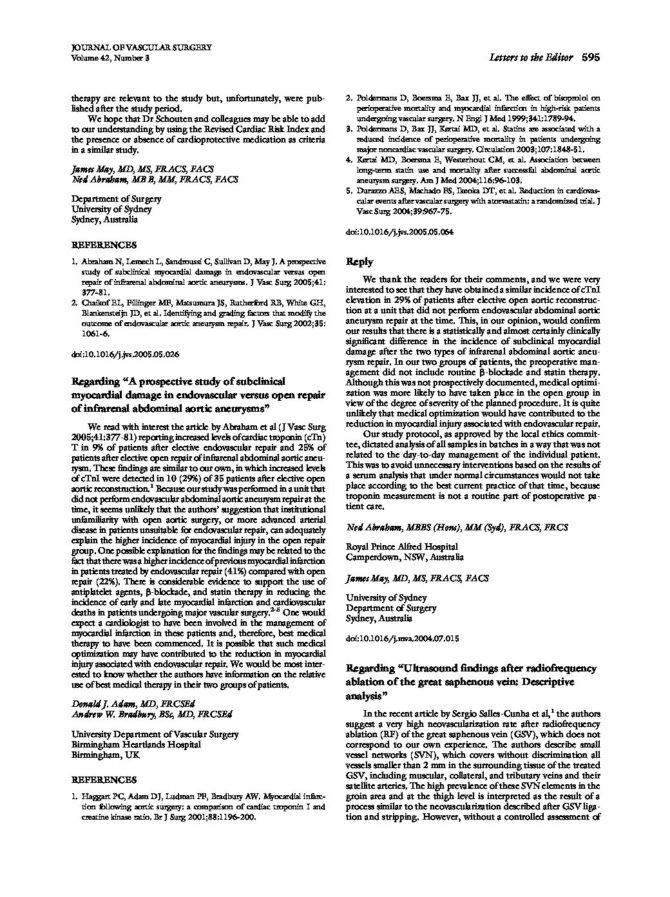
In fact, many small vessels can be identified with ultrasonography before any treatment, and there is no reason that RF ablates them. For example, the external pudendal artery visible in contact with the GSV termination in preoperative ultrasound examination remains discernible after RF, in contact with the occluded GSV. Similarly, it is common to visualize arterioles close to the GSV during ultrasonography-guided sclerotherapy (Figure). Considering these arterioles as SVN, they cannot be attributed to neovascularization. Regarding the veins, it is known that the saphenofemoral junction (SFJ) tributaries, which are also covered by the SVN definition, remain patent after RF in more than 90% of cases.1
Therefore, it is not surprising that the authors found a lower prevalence of SVN when a high ligation was performed. It would have been helpful for the authors to provide a more anatomically precise SVN classification. It is difficult to assign an identical pathologic effect to vessels so anatomically different as arterioles and refluxing or not refluxing veins. In our experience, refluxing veins observed after RF—excepting the cases of recanalization or nonocclusion—involve only the low SFJ tributaries or the groin ganglionic veins.
The persistence of a short patent segment at the termination of the GSV is a known pattern, consistent with the endovenous therapeutic concept that allows physiologic drainage of the SFJ collaterals toward the deep system.2 However, the prognosis of GSV termination recanalization in case of associated high ligation should be more pejorative because of the possibility of physiologic drainage of the recanalized GSV is suppressed. The rate of GSV trunk recanalization in this study (35%) is much higher than previously reported (9.5% at 2 years and 11.5% at 4 years).2,3 Knowing that only 20% of the GSVs with partial occlusion or nonocclusion are refluxing, it is not obvious that the network including the feeding vein, the recanalized GSV, and the draining vein observed by the authors was inconsistent with a physiologic circulation, especially in the absence of reflux. Because the endovenous treatment concept is very different from conventional surgery, it is mandatory to attentively assess the results of RF. Ensuring an identical preoperative and postoperative ultrasound method to establish consistent conclusions is also necessary.

Pretreatment duplex image showing collateral veins and arteries close to the refluxing great saphenous vein (GSV) trunk.
REFERENCES
- Salles-Cunha SX, Comerota AJ, Tzilinis A, Dosick SM, Gale SS, Seiwert AJ, et al. Ultrasound findings after radiofrequency ablation of the great saphenous vein: descriptive analysis. J Vasc Surg 2004;40:1066-73.
- Pichot O, Kabnick LS, Creton D, Merchant RF, Schuller-Petrovic S, Chandler JG. Duplex ultrasound scan findings two years after great saphenous vein radiofrequency endovenous obliteration. J Vasc Surg 2004;39:189-95.
- Merchant RF, Pichot O, Myers KA. Four-year follow-up on endovascular radiofrequency obliteration of great saphenous reflux. Dermatol Surg 2005;31:129-34.
| Date | 2005 |
| Auteurs | J Vasc Surg 2005;42:595-97 letter to the editor PICHOT O, CRETON D. |